Allergic rhinitis continues to exact a high toll on the quality of life of Americans, according to a survey presented here at the American Academy of Allergy, Asthma and Immunology (AAAAI) 2011 Annual Meeting.
"The data are timely, as they were collected from patients who have allergies in surveys less than 1 year ago," study presenter Gary Gross, MD, from the Dallas Allergy and Asthma Center, Texas, told Medscape Medical News. "The results are more of a stimulus to try to improve the care for these patients whose lives are so dramatically influenced by allergies."
Reached for comment, Neeta Ogden, MD, an adult and pediatric allergist at Englewood Hospital and Medical Center in New Jersey, and member of the AAAAI, noted that "the quality-of-life impact can be overlooked in clinical practice."
"People may think allergies are not as 'life-threatening' as other medical problems like diabetes or high blood pressure, etc. However, untreated allergies, especially during the peak pollen months, can lead to daily impairment that affects work/school and quality of life," Dr. Ogden said.
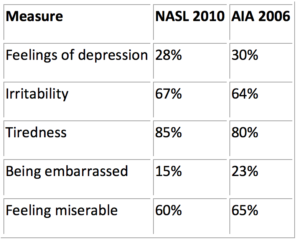
Comparative Look at NASL 2010 and AIA 2006
At the AAAAI's annual gathering, Dr. Gross presented results of the 2010 Nasal Allergy Survey Assessing Limitations (NASL) Survey, looking at the effect allergic rhinitis currently has on the quality of life of Americans.
As part of the survey, 400 people aged 18 years and older who had been diagnosed with allergic rhinitis and who had experienced nasal allergy symptoms or taken medication for their condition in the past 12 months were interviewed. The findings were compared with 2500 respondents from the 2006 Allergies in America Survey (AIA) to determine the degree to which allergic rhinitis still affects patient quality of life.
A look at the 2 data sets suggests no apparent easing of the emotional toll of allergic rhinitis, the researchers say.
Table. Comparison Between NASL 2010 and AIA 2006
"The survey reminds us all that these patients suffer far beyond the congestion, runny nose, and sneezing that are characteristic symptoms of allergic rhinitis, and that they need more effective treatment to be productive and to improve their quality of life," Dr. Gross told Medscape Medical News.
He advised clinicians to "question patients who have allergic rhinitis more thoroughly regarding how allergic rhinitis impacts the quality of the patients' lives, and then try to determine the best approach to treatment."
The NASL 2010 survey also confirms that allergic rhinitis limits peoples' ability to participate in social activities (29%), to have or play with pets (34%), and to participate in outdoor (52%) and indoor (13%) activities.
Mirroring the AIA 2006 survey, 33% of respondents in NASL 2010 reported their symptoms affected them "a lot" or a "moderate" amount during the month when nasal symptoms were at their worst. In NASL 2010, work productivity was roughly 71% when nasal symptoms were at their worst; the figure was nearly the same (72%) among AIA 2006 respondents.
Nasal symptoms of allergic rhinitis also contribute to "substantial" sleep disturbances, including trouble falling to sleep and staying asleep, according to other data from the NASL 2010 Survey reported separately at the meeting.
New Data "Not Surprising"
In Dr. Ogden's view, the NASL 2010 findings are "not surprising, especially since allergy symptoms seem to be more intense than ever and people are experiencing new-onset allergies and worsening of existing allergies in the last few years."
"In terms of seasonal allergies," she said, "this has been attributed to global warming leading to more intense, longer seasons. People seem to have worse symptoms and often express breakthrough allergy symptoms even on doses of medications that used to help them before."
Following up with patients is key, Dr. Ogden said, "because there are a number of therapies out there that can be added if the first medication doesn't work. In addition, getting patients on your and their own radar in terms of allergy so they can start medications 2 to 3 weeks before the peak season is also important."
Dr. Gross and Dr. Ogden have disclosed no relevant financial relationships.
American Academy of Allergy, Asthma and Immunology 2011 Annual Meeting: Abstract 838. Presented March 20, 2011.
Source: http://www.medscape.com/viewarticle/739928 Megan Brooks







Join the conversation